Mary K. Wakefield.
Mary
Wakefield, Ph.D., R.N., F.A.A.N. Associate Dean for Rural Health and
Director, Center for Rural Health; School of Medicine and Health
Sciences; University of North Dakota; Grand Forks, ND. E-mail: mwake@medicine.nodak.edu
Exhaustive
research documents the fact that today in America, there is no
guarantee that any individual will receive high-quality care for any
particular health problem. Health care is plagued with inappropriate
utilization of health services and errors in health care practice.1
The quality and safety of health care in this nation were assessed
through a series of 11 reports from the Institute of Medicine (IOM).
Some of the most significant components of the first two reports are a
set of aims to achieve high-quality care and new rules to guide the
redesign of the broken health care system. The needed transformation and
steps to achieving redesign are substantial because the chasm between
what currently exists in health care and what should exist to achieve
high-quality care is sizeable. While only four of the IOM reports will
be discussed in this section—other reports are discussed in other
chapters later in this book—each has significant implications for
nursing and for how care should be delivered.
In 1999, the IOM released its landmark report, To Err Is Human: Building a Safer Health System.2 The chilling conclusion of that report was that thousands of people were injured by the very health system from which they sought help. Tens of thousands of Americans die each year and hundreds of thousands are injured. That report and its companion, Crossing the Quality Chasm,3 have had a profound impact on how health care is viewed. The information and perspectives moved conversations regarding patient safety and quality care from inside health care institutions to the mainstream of media, corporate America, and public policy. The reports raised awareness of the depth and complexity of quality challenges and prompted the marked expansion of quality improvement efforts through research and other means.
The most significant barrier to improving patient safety identified in To Err Is Human is a “lack of awareness of the extent to which errors occur daily in all health care settings and organizations. This lack of awareness exists because the vast majority of errors are not reported, and errors are not reported because personnel fear they will be punished”2 (p. 155). While these statements describing the essence of the challenges facing health care are simple and straightforward, the level and complexity of effort needed to address them is not. Since the release of the two reports, broad-based efforts have begun to bring more sophistication and precision to measuring and improving the safety and quality of health care. Nevertheless, substantial work in both academic and practice settings remains to be done.
While the IOM reports initiated tectonic shifts in attention and effort, the reports were not the first set of clear statements of concern regarding safety and quality. Nor were these reports the first efforts at calling attention to the need for data, public reporting, and the consideration of health care quality in light of payment for care. More than 140 years earlier, Florence Nightingale, the founder of modern nursing, raised these same issues. In spite of the passage of well over a century between Nightingale and the release of the IOM reports, seemingly little attention was paid in the interim to creating safer health care environments.
Three comparisons of Nightingale’s concerns and recommendations with those expressed in the IOM reports illustrate similar problem identification as well as a shared view regarding the building blocks essential to creating solutions. First, in her publication, Notes on Hospitals,4 Nightingale identified the paradox of the problem at hand: “In practice a hospital may be found only to benefit a majority, and to inflict suffering on the remainder” (p. 20). Well over a century later, To Err Is Human says, “… a person … should not have to worry about being harmed by the health system itself”2 (p. 5). Nightingale goes on to say, “Even admitting to the full extent the great value of hospital improvements of recent years, a vast deal of suffering, and some at least of the mortality, in these establishments is avoidable”4 (p. 3). Similarly, To Err Is Human notes, “A substantial body of evidence points to medical errors as a leading cause of death and injury”2 (p. 26).
Finally, in a search for solutions and with an eye toward measurement, developing evidence, public reporting, and linking payment with quantifiable performance, Nightingale advances4 (p. 3), “It is impossible to resist the conviction that the sick are suffering from something quite other than the disease inscribed on their bed ticket—and the inquiry … arises in the mind, what can be the cause?” Related to this, To Error Is Human notes, “Sufficient attention must be devoted to analyzing and understanding the causes of errors in order to make improvements”2 (p. 87). In addition, the report notes, “Group purchasers have the ability to consider safety issues in their contracting decisions”2 (p. 152).
As is evident in the similarity of statements between Nightingale and the IOM, concerns about medical error and compromises in patient safety bridge a significant passage of time. It is difficult not to speculate about what safety in health care would look like today had Nightingale’s calls to action been heeded. Rather than lagging behind, health care in the 21st century might have been the leader in safety among high-risk industries such as aviation and nuclear power production. Instead, clinicians, policymakers, and many others search for safety and quality lessons to apply in health care delivery from these and other high-risk but safer industries. Irony exists in that these industries, nonexistent during Nightingale’s time, have made substantially more progress than health care in creating safe environments.
In 1999, the IOM released its landmark report, To Err Is Human: Building a Safer Health System.2 The chilling conclusion of that report was that thousands of people were injured by the very health system from which they sought help. Tens of thousands of Americans die each year and hundreds of thousands are injured. That report and its companion, Crossing the Quality Chasm,3 have had a profound impact on how health care is viewed. The information and perspectives moved conversations regarding patient safety and quality care from inside health care institutions to the mainstream of media, corporate America, and public policy. The reports raised awareness of the depth and complexity of quality challenges and prompted the marked expansion of quality improvement efforts through research and other means.
The most significant barrier to improving patient safety identified in To Err Is Human is a “lack of awareness of the extent to which errors occur daily in all health care settings and organizations. This lack of awareness exists because the vast majority of errors are not reported, and errors are not reported because personnel fear they will be punished”2 (p. 155). While these statements describing the essence of the challenges facing health care are simple and straightforward, the level and complexity of effort needed to address them is not. Since the release of the two reports, broad-based efforts have begun to bring more sophistication and precision to measuring and improving the safety and quality of health care. Nevertheless, substantial work in both academic and practice settings remains to be done.
While the IOM reports initiated tectonic shifts in attention and effort, the reports were not the first set of clear statements of concern regarding safety and quality. Nor were these reports the first efforts at calling attention to the need for data, public reporting, and the consideration of health care quality in light of payment for care. More than 140 years earlier, Florence Nightingale, the founder of modern nursing, raised these same issues. In spite of the passage of well over a century between Nightingale and the release of the IOM reports, seemingly little attention was paid in the interim to creating safer health care environments.
Three comparisons of Nightingale’s concerns and recommendations with those expressed in the IOM reports illustrate similar problem identification as well as a shared view regarding the building blocks essential to creating solutions. First, in her publication, Notes on Hospitals,4 Nightingale identified the paradox of the problem at hand: “In practice a hospital may be found only to benefit a majority, and to inflict suffering on the remainder” (p. 20). Well over a century later, To Err Is Human says, “… a person … should not have to worry about being harmed by the health system itself”2 (p. 5). Nightingale goes on to say, “Even admitting to the full extent the great value of hospital improvements of recent years, a vast deal of suffering, and some at least of the mortality, in these establishments is avoidable”4 (p. 3). Similarly, To Err Is Human notes, “A substantial body of evidence points to medical errors as a leading cause of death and injury”2 (p. 26).
Finally, in a search for solutions and with an eye toward measurement, developing evidence, public reporting, and linking payment with quantifiable performance, Nightingale advances4 (p. 3), “It is impossible to resist the conviction that the sick are suffering from something quite other than the disease inscribed on their bed ticket—and the inquiry … arises in the mind, what can be the cause?” Related to this, To Error Is Human notes, “Sufficient attention must be devoted to analyzing and understanding the causes of errors in order to make improvements”2 (p. 87). In addition, the report notes, “Group purchasers have the ability to consider safety issues in their contracting decisions”2 (p. 152).
As is evident in the similarity of statements between Nightingale and the IOM, concerns about medical error and compromises in patient safety bridge a significant passage of time. It is difficult not to speculate about what safety in health care would look like today had Nightingale’s calls to action been heeded. Rather than lagging behind, health care in the 21st century might have been the leader in safety among high-risk industries such as aviation and nuclear power production. Instead, clinicians, policymakers, and many others search for safety and quality lessons to apply in health care delivery from these and other high-risk but safer industries. Irony exists in that these industries, nonexistent during Nightingale’s time, have made substantially more progress than health care in creating safe environments.
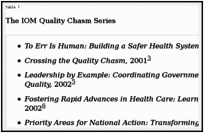
Since the release of To Err Is Human and Crossing the Quality Chasm, the IOM has produced 9 additional related reports. The IOM Quality Chasm Series (see Table 1)
includes reports linking quality to a range of issues, from health
professions education, to health care in rural America, to improving
health care quality for mental health and substance-abuse systems.
Threaded through this series are key concepts of the framework presented
in the original two reports. In each report, facets of the framework
are expanded or applied to specific populations or system
characteristics. The language of most of the reports tends to group
members of health care disciplines by the terms “providers” or
“clinicians,” with an occasional mention of specific professional groups
such as medicine or nursing. Generally speaking, the content of the
reports are directly or indirectly applicable to all health care
professionals. Consequently, each of the 11 reports has implications for
aspects of nursing practice, research, education, and public policy
engagement.
 This
section focuses on nursing implications associated with selected
issues, concepts, findings, and recommendations specifically embedded in
4 of the 11 reports: To Err Is Human, Crossing the Quality Chasm, Health Professions Education: A Bridge to Quality, and Quality Through Collaboration: The Future of Rural Health Care
(often referred to as the rural report). The identified nursing
implications in these four reports give a sense of the relevance and
utility of these reports to the nursing discipline. The first two
reports discussed in this chapter established the scope of the problems
associated with compromises in quality of health care and offered a
framework for addressing those problems. The third report, on health
professions education, described the critical role health professions
education plays in facilitating or impeding the delivery of consistent,
high-quality health care. The nursing profession, central to health care
delivery, is a pivotal audience for this report.
This
section focuses on nursing implications associated with selected
issues, concepts, findings, and recommendations specifically embedded in
4 of the 11 reports: To Err Is Human, Crossing the Quality Chasm, Health Professions Education: A Bridge to Quality, and Quality Through Collaboration: The Future of Rural Health Care
(often referred to as the rural report). The identified nursing
implications in these four reports give a sense of the relevance and
utility of these reports to the nursing discipline. The first two
reports discussed in this chapter established the scope of the problems
associated with compromises in quality of health care and offered a
framework for addressing those problems. The third report, on health
professions education, described the critical role health professions
education plays in facilitating or impeding the delivery of consistent,
high-quality health care. The nursing profession, central to health care
delivery, is a pivotal audience for this report.
The Future of Rural Health Care addresses the long-standing lack of attention brought to rural health care quality in spite of the fact that between one-fourth and one-fifth of the population resides in rural America. This report sheds light on the unique features of rural health care and tailored approaches to addressing quality shortcomings. Particularly relevant to nurses, however, is that The Future of Rural Health Care introduced innovative approaches that move beyond health care and focus on the quality of the health of populations. Whether viewed from a rural or urban context, the latter orientation is an important focus for nurses to consider in their future work and research.
Table 1
The IOM Quality Chasm Series
The Future of Rural Health Care addresses the long-standing lack of attention brought to rural health care quality in spite of the fact that between one-fourth and one-fifth of the population resides in rural America. This report sheds light on the unique features of rural health care and tailored approaches to addressing quality shortcomings. Particularly relevant to nurses, however, is that The Future of Rural Health Care introduced innovative approaches that move beyond health care and focus on the quality of the health of populations. Whether viewed from a rural or urban context, the latter orientation is an important focus for nurses to consider in their future work and research.
As the first report in the IOM Quality Chasm series, To Err Is Human
frames the scope of the challenge for improving safety in health care
systems. Safety is defined as freedom from accidental injury.2
Articulated in the report is the heavy toll associated with safety
compromises and health care errors in terms of human lives, suffering,
and financial burden of health care services. Financial burden is borne
by individuals, employers, insurance companies, and governmental
programs such as Medicare and Medicaid. Approximately 30 research
studies were reviewed and established the evidence base for the IOM’s
Committee on Quality of Health Care in America determination that error
is a cause of very significant and widespread injury and mortality. Many
of the research studies focused on activities that incorporated nursing
functions such as medication processes. Additionally, a number of the
reviewed studies helped to illuminate the predeterminants of error.
Due to the dearth of evidence to serve as the basis for some of the conclusions and recommendations in this report, the IOM acknowledged that current understanding of the epidemiology of errors was fragmented. Calls for research efforts were evident throughout the report. “Research and analysis are not luxuries in the operation of safety systems. They are essential steps in the effective redesign of systems”2 (p. 181). Clearly there is opportunity for nurse researchers, along with others, to make significant and important contributions to address this knowledge deficit with needed evidence.
In addition to increasing awareness of the scope and significance of medical errors, a set of strategies and recommendations were advanced to encourage patient safety and quality improvement. Major emphasis is placed on (1) the essential role of leadership in addressing errors, (2) the need for and structure of error reporting systems, (3) the development of performance standards, and (4) recommendations regarding elements key to safety design in health care systems. The committee producing the report devoted considerable attention to making the case that perfection based on human performance—while a long-standing expectation of the work of nurses, physicians, and others—is both faulty and dangerous. In reorienting expectations from a focus on individuals to a focus on systems, the report clearly and firmly stated that to eliminate the source of a vast majority of errors and near misses, health care systems must be designed to make it very hard for nurses and others to make errors. This orientation runs directly counter to long-held views by both the public and health care providers themselves: that mistakes are solely the result of individual provider actions and that blame should be assigned accordingly. The report refocused attention on the need to construct systems that make it easy for nurses and others to engage in safe practices and difficult to execute actions that are unsafe.
Accrediting organizations influence nursing care quality through their safety and quality standards. Highly influential in this regard has been the marked expansion of safety expectations of accrediting bodies, such as the Joint Commission (formerly known as the Joint Commission on Accreditation of Healthcare Organizations [JCAHO]). The Joint Commission National Patient Safety Goals (NPSGs) are very prescriptive and explicit in their impact on aspects of nursing practice. For example, the Joint Commission’s safety goals include standardizing handoff communications, including an opportunity to ask and respond to questions, and a goal to encourage the active involvement of patients and their families in the patient’s care as a patient safety strategy14 (e.g., patient- and family-centered care).
External drivers also include steps being taken by the Centers for Medicare and Medicaid Services to link reporting performance on quality indicators with payment. These payment changes reward hospitals that publicly report their performance on a predetermined set of quality indicators, many of which are directly or indirectly influenced by nursing actions. Private sector entities such as insurance companies are moving in similar directions. The intense interest in aligning payment with performance (i.e., health sector income and patient outcome) has significant implications for nursing. Put simply, maintaining and strengthening the financial health of hospitals and other segments of the health care delivery system is linked in no small part to the practice of nursing in these facilities. Consequently, alignment of reimbursement with quality is redirecting the attention of health care administrators. To the extent that research continues to link nursing practices, staffing, and other characteristics (e.g., educational background and number of hours worked) to the quality of patient care, nursing will be positioned to receive considerably more attention from health care system leadership.
Recognizing that more could be done to improve patient outcomes the report called for the incorporation of patient safety considerations into clinical practice guidelines, as well as the development of guidelines specifically focused on patient safety. Particular attention is paid to the need for engaging interdisciplinary approaches to guideline development. Nurses’ expertise and functions clearly overlap with a number of other disciplines in particular content areas (e.g., mental health care and critical care). This overlap makes this recommendation difficult to pursue, but appropriate to nursing as well as other disciplines. Nursing education, as well as State and national nursing organizations, can expand efforts to engage interdisciplinary partners in developing shared academic curricula and conference and meeting content. Additionally, nurse clinicians, researchers, and others should further the development of safety aspects of clinical guidelines development in concert with representatives of other health care disciplines.
Another report recommendation called for professional organizations to firmly commit to an agenda focused on patient safety, with specific efforts targeted toward health professions education. Efforts can emerge through curriculum development, the inclusion of safety content on conference agendas, and ongoing in-service education. Various nursing organizations have responded to aspects of this recommendation. However, in light of many competing priorities, expanding and sustaining this focus over time and across multiple venues will challenge nurses and the nursing profession.
The final external driver addressed in the report addressed whether or not the public is engaged in safety improvement efforts. Professional organizations, particularly those that represent nurses, can help to accomplish this by working with both the public and policymakers. Some national nursing organizations already have made safety part of their public policy agenda (e.g., the Association of Operating Room Nurses). Nevertheless, there is substantial work that could occur to create new efforts that educate and engage the broader public in health care safety activities. As a profession, nursing commands considerable trust from the American public. Also, nursing places high value on the importance of educating individuals, families, and communities about health and health care in order to fully engage them as partners in their health. Consequently, nurses are particularly well positioned to engage in the challenging work of assisting the public to understand both the complexity of patient safety and error, and the actions they can engage in to help ensure they receive safe health care. Individual nurses can engage this type of effort in concert with other health team members. This work can also be done through nursing organizations and in tandem with insurers, employers, and others who recognize the pivotal role health care consumers can play in ensuring the delivery of safe care.
Due to the dearth of evidence to serve as the basis for some of the conclusions and recommendations in this report, the IOM acknowledged that current understanding of the epidemiology of errors was fragmented. Calls for research efforts were evident throughout the report. “Research and analysis are not luxuries in the operation of safety systems. They are essential steps in the effective redesign of systems”2 (p. 181). Clearly there is opportunity for nurse researchers, along with others, to make significant and important contributions to address this knowledge deficit with needed evidence.
In addition to increasing awareness of the scope and significance of medical errors, a set of strategies and recommendations were advanced to encourage patient safety and quality improvement. Major emphasis is placed on (1) the essential role of leadership in addressing errors, (2) the need for and structure of error reporting systems, (3) the development of performance standards, and (4) recommendations regarding elements key to safety design in health care systems. The committee producing the report devoted considerable attention to making the case that perfection based on human performance—while a long-standing expectation of the work of nurses, physicians, and others—is both faulty and dangerous. In reorienting expectations from a focus on individuals to a focus on systems, the report clearly and firmly stated that to eliminate the source of a vast majority of errors and near misses, health care systems must be designed to make it very hard for nurses and others to make errors. This orientation runs directly counter to long-held views by both the public and health care providers themselves: that mistakes are solely the result of individual provider actions and that blame should be assigned accordingly. The report refocused attention on the need to construct systems that make it easy for nurses and others to engage in safe practices and difficult to execute actions that are unsafe.
External Drivers of Safety and Quality
The report described external drivers that can improve the safety and quality of health care, including nursing care. External drivers that influence the quality of nursing care included regulation and legislation, accrediting organizations, efforts to link payment with performance, the need for interdisciplinary guidelines, the commitment of professional organizations, and the level of public engagement. The report included a number of observations about the role that licensing and credentialing processes can have in building appropriate performance standards and expectations for all health professionals. Examples of regulation and legislation that impact nursing care quality included State scope-of-practice laws that govern what nurses are legally licensed to do and stipulate performance expectations. Subsequently, there are concerns about whether current methods of licensing and credentialing adequately assess the safety and competence of skills across health professionals, including nurses. More than 20 States now have laws requiring error reporting, and with recent Federal reporting legislation, serious errors that reflect nursing and other care processes are now governed by reporting expectations from outside the health care system.Accrediting organizations influence nursing care quality through their safety and quality standards. Highly influential in this regard has been the marked expansion of safety expectations of accrediting bodies, such as the Joint Commission (formerly known as the Joint Commission on Accreditation of Healthcare Organizations [JCAHO]). The Joint Commission National Patient Safety Goals (NPSGs) are very prescriptive and explicit in their impact on aspects of nursing practice. For example, the Joint Commission’s safety goals include standardizing handoff communications, including an opportunity to ask and respond to questions, and a goal to encourage the active involvement of patients and their families in the patient’s care as a patient safety strategy14 (e.g., patient- and family-centered care).
External drivers also include steps being taken by the Centers for Medicare and Medicaid Services to link reporting performance on quality indicators with payment. These payment changes reward hospitals that publicly report their performance on a predetermined set of quality indicators, many of which are directly or indirectly influenced by nursing actions. Private sector entities such as insurance companies are moving in similar directions. The intense interest in aligning payment with performance (i.e., health sector income and patient outcome) has significant implications for nursing. Put simply, maintaining and strengthening the financial health of hospitals and other segments of the health care delivery system is linked in no small part to the practice of nursing in these facilities. Consequently, alignment of reimbursement with quality is redirecting the attention of health care administrators. To the extent that research continues to link nursing practices, staffing, and other characteristics (e.g., educational background and number of hours worked) to the quality of patient care, nursing will be positioned to receive considerably more attention from health care system leadership.
Recognizing that more could be done to improve patient outcomes the report called for the incorporation of patient safety considerations into clinical practice guidelines, as well as the development of guidelines specifically focused on patient safety. Particular attention is paid to the need for engaging interdisciplinary approaches to guideline development. Nurses’ expertise and functions clearly overlap with a number of other disciplines in particular content areas (e.g., mental health care and critical care). This overlap makes this recommendation difficult to pursue, but appropriate to nursing as well as other disciplines. Nursing education, as well as State and national nursing organizations, can expand efforts to engage interdisciplinary partners in developing shared academic curricula and conference and meeting content. Additionally, nurse clinicians, researchers, and others should further the development of safety aspects of clinical guidelines development in concert with representatives of other health care disciplines.
Another report recommendation called for professional organizations to firmly commit to an agenda focused on patient safety, with specific efforts targeted toward health professions education. Efforts can emerge through curriculum development, the inclusion of safety content on conference agendas, and ongoing in-service education. Various nursing organizations have responded to aspects of this recommendation. However, in light of many competing priorities, expanding and sustaining this focus over time and across multiple venues will challenge nurses and the nursing profession.
The final external driver addressed in the report addressed whether or not the public is engaged in safety improvement efforts. Professional organizations, particularly those that represent nurses, can help to accomplish this by working with both the public and policymakers. Some national nursing organizations already have made safety part of their public policy agenda (e.g., the Association of Operating Room Nurses). Nevertheless, there is substantial work that could occur to create new efforts that educate and engage the broader public in health care safety activities. As a profession, nursing commands considerable trust from the American public. Also, nursing places high value on the importance of educating individuals, families, and communities about health and health care in order to fully engage them as partners in their health. Consequently, nurses are particularly well positioned to engage in the challenging work of assisting the public to understand both the complexity of patient safety and error, and the actions they can engage in to help ensure they receive safe health care. Individual nurses can engage this type of effort in concert with other health team members. This work can also be done through nursing organizations and in tandem with insurers, employers, and others who recognize the pivotal role health care consumers can play in ensuring the delivery of safe care.
Principles for the Design of Safe Systems
Internal drivers that impact the safety and quality of care include policies, management decisions, and other organizational features that either help to prevent or predispose individuals to committing errors. The IOM report identified internal drivers as being most hazardous to safety in complex systems (e.g., health care), because generally speaking, the internal drivers’ influence on error is not readily apparent.2 Applied to nursing, quality and safety are products of interactions between nurses and others, between nurses and technology, and between nurses and care processes. To address threats to quality and safety by internal drivers, five principles for the design of safe systems are articulated in To Err Is Human, each of which has direct relevance to nursing practice.- Principle
1: The commitment of senior level managers and leaders of health care
institutions is essential to moving a quality and safety agenda forward
in care settings.
Nurse leaders, in tandem with other institutional leaders, have a role in ensuring that patient safety is a priority corporate objective, a responsibility shared by everyone, and that expectations for safety oversight are clearly articulated and assigned. Efforts directed toward highlighting the importance and expectations of the quality and safety agenda need to reach up to boards of directors and across to all employees within health care settings. Nursing leadership has a core responsibility to help ensure that this orientation is pervasive within the institution and that it is firmly embraced by the senior ranks of the organization. - Principle
2: Human limits in care processes need to be explicitly identified and
strategies put in place to minimize the likelihood that these
limitations are expressed in the work environment.
Nurses should be attuned to determining and addressing sources of potential error. Protocols and checklists that help guide nursing actions should be readily available and used. Determining ways to simplify processes, such as reducing the number of handoffs and standardizing actions, devices, or doses to minimize the likelihood of error, should involve all nurses. - Principle 3: Effective team functioning,
promoted and fostered by the institution, is an essential component of
health care systems that are quality and patient safety driven.
This includes team training approaches as well as involving patients in safety design and care processes. Features of this principle are more fully developed in the IOM report, Health Professions Education: A Bridge to Quality, and will be discussed in that section. - Principle
4: The redesign of systems for safe care involves anticipating the
unexpected and adopting proactive approaches to ensuring safe care.
This principle covers such important attributes as improving access to accurate and timely information and designing for recovery. Since the release of To Err Is Human, specific evidence-based activities designed to anticipate the unexpected are being implemented. For example, the deployment of rapid response teams in health care environments is designed to prevent serious adverse events such as cardiac or respiratory arrest.15 With the help of nursing knowledge and research, other equally important high-impact care processes will be developed over time. - Principle
5: Creating a learning environment addresses the extremely complex work
of changing organizational and academic cultures so that error is
viewed as an opportunity to learn.
A learning environment does not seek to fix blame, but ensures that reporting systems have well-developed approaches for communicating how identified problems will be addressed. Also important, given the historical power gradient among nurses and physicians and others, is the free flow of information without the inhibiting hierarchies.2 Learning environments ensure that all staff have high comfort levels in communicating any and all safety concerns. Some of the most complex patient safety work involves creating organizational cultures and expectations that embrace these features. Redesigning the education of the next generation of nurses so they are capable of maximizing their contributions in these environments is a necessary component.
Nurse leaders should play key roles in ensuring that patient safety programs inside health care organizations are highly visible, implement nonpunitive reporting processes, and incorporate safety principles into daily practice, all of which are called for in the recommendations of To Err Is Human. The second report, Crossing the Quality Chasm, describes at greater length the use of internal and external approaches to meaningfully improve the quality of health care.
Broader quality challenges described in Crossing the Quality Chasm3 are equal to patient safety in their complexity. While the entire Quality Chasm
report is highly relevant to nursing concerns, only a small set of key
concepts with implications for nursing will be presented here. This
discussion is for the purpose of illustrating the implications of this
report for the nursing profession, and to highlight ways that nurses
individually and collectively can align their efforts with the content
of these highly regarded reports. Challenges to quality are divided into
three types: (1) overuse, which refers to the application of health
care services where the potential for harm exceeds the potential for
benefit; (2) underuse, which is the absence of a service when it is
indicated; and (3) misuse, which is in the provision of an appropriate
service, a preventable injury occurs.3
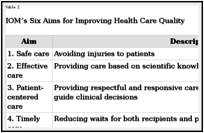
The Quality Chasm report described the work of health care as being “characterized by more to know, more to manage, more to watch, more to do, and more people involved in doing it at any time in the nation’s history”3 (p. 25). The statement is certainly descriptive of nursing as well. All too familiar to nurses is the growing complexity of both health care and the nature of nursing knowledge and nursing practice. Given these complexities, individual nurses, as with other clinicians, cannot possibly recall and apply all knowledge necessary for the delivery of safe, high-quality patient, family, or community care. The complexity of nursing and medical practice has markedly increased, the technologies are more numerous and complex, and the evidence base underlying practice is rapidly expanding. Recognizing these challenges, the first recommendation in the Quality Chasm report restated the purpose of the health care system as articulated by President Clinton’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry: “All health care organizations, professional groups, and private and public purchasers should adopt as their explicit purpose to continually reduce the burden of illness, injury and disability, and to improve the health and functioning of the people of the United States.”3 (p. 39). In contemplating this statement, nurses might ask what the collective contribution of nursing is and should be to achieving this purpose. How do we pursue this goal? How do we know whether we and other stakeholders in the U.S. health care system are making progress toward achieving it? The Quality Chasm report adds more specificity to this recommendation by setting out six aims (see Table 2). To achieve the aims of the purpose statement articulated above, the Quality Chasm report suggests that these six aims should be the focus of nurses and other clinicians, and should be pursued in all health care settings.
 Illustrations of the relevance and integral nature of nursing to achieving these aims are illustrated below.
Illustrations of the relevance and integral nature of nursing to achieving these aims are illustrated below.
In addition to expecting the further development of and adherence to an evidence base, the Quality Chasm report also highlights the importance of nurses and other clinicians systematically and continually reviewing the outcomes of the care that they provide. Currently, care results are rolled up and reflected in overall performance indicators for nursing homes and hospitals. With some exceptions, there is relatively limited information that is currently collected, assessed, and fed back to nurses to help them better understand their individual impact on care quality and thereby assist them in improving their performance. Clearly, efforts that have resulted in the development of nursing indicators are a step in this direction. This is one more important area in which nurses can engage to further the quality improvement agenda.
Efforts to improve timeliness are multifaceted. One of the essential tools to address parts of this challenge is technology. The expanded use of call-a-nurse lines, e-mail exchanges between clinicians and patients, and consumer access to telemedicine applications linking rural and urban facilities, are part of the developing technology-based toolkit needed to increase timely access to care.
Additionally, nurse researchers can play an exceedingly important role in achieving efficiency. For example, Naylor17 found that elderly patients receiving a comprehensive intervention delivered by advanced practice nurses (APNs) in the hospital and followed in the home significantly decreased expensive hospitalizations. APN care resulted in average per capita expenditures of $6,152 compared to the control group expenditure of $9,618. As a result, efforts are underway to help move this intervention into the broader practice environment.
As the growth in health care expenditures continues to rise nationally, public policymakers, insurers, and others will be far more open to nursing practice models as well as other strategies that help to rein in high costs while sustaining or improving care quality. Efforts toward achieving this aim provide new opportunities for nurses to create models that maximize the contribution of nursing care and innovation in quality improvement.
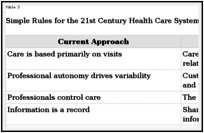 As
with the aims for improvement, implementing this entire set of rules in
the redesign of health care systems has implications for nursing
practice, education, and research. While nursing can be considered in
the context of each of the current and new rules, only a few of the
rules are discussed here in order to illustrate their relevance to
nursing. For example, operationalizing the first new rule, care based on
continuous healing relationships, focuses on ensuring that patients
have the care they need when they need it. Continuity and coordination
should trump fragmented, disconnected care efforts. Conceivably, this
rule could directly influence where, how, and when nursing care is
available to patients. Moreover, the Internet is likely to play a
pivotal role in its application. Another example, the third rule—the
patient is the source of control—is designed to facilitate
decisionmaking by patients rather than authoritarian or paternalistic
decisionmaking by health care providers. While often considered in the
context of physician-patient communication, this rule has implications
for the approaches nurses bring to patient engagement. However, in
addition to individual nurse efforts to incorporate this orientation
into patient care, major system-level changes will be needed to allow
patients to exercise their preferred degree of control. Such
system-level redesign, particularly as it relates to nurse-patient
interactions, will benefit from nursing input.
As
with the aims for improvement, implementing this entire set of rules in
the redesign of health care systems has implications for nursing
practice, education, and research. While nursing can be considered in
the context of each of the current and new rules, only a few of the
rules are discussed here in order to illustrate their relevance to
nursing. For example, operationalizing the first new rule, care based on
continuous healing relationships, focuses on ensuring that patients
have the care they need when they need it. Continuity and coordination
should trump fragmented, disconnected care efforts. Conceivably, this
rule could directly influence where, how, and when nursing care is
available to patients. Moreover, the Internet is likely to play a
pivotal role in its application. Another example, the third rule—the
patient is the source of control—is designed to facilitate
decisionmaking by patients rather than authoritarian or paternalistic
decisionmaking by health care providers. While often considered in the
context of physician-patient communication, this rule has implications
for the approaches nurses bring to patient engagement. However, in
addition to individual nurse efforts to incorporate this orientation
into patient care, major system-level changes will be needed to allow
patients to exercise their preferred degree of control. Such
system-level redesign, particularly as it relates to nurse-patient
interactions, will benefit from nursing input.
Regarding new rule four, shared knowledge and free flow of information, Quality Chasm cited evidence that giving patients access to their own health and clinical information improves care processes and health outcomes. Clearly, electronic personal health records and Web-based information have considerable potential to enhance patient knowledge and stimulate healthy behavior. However, there is limited information about how nurses can help patients to fully harness these information resources. Nurses can lead efforts to make these rules actionable across health systems, particularly as they influence the redesign of nursing practice, the nurse-patient relationships, the relationships between nurses and other disciplines, and the relationship of nurses to care processes. Additionally, these expectations should be incorporated into nursing curricula to ensure that nurses are able to engage and support the refinement and application of important features of redesigned health care systems. In the process, nurses learn not just the changes necessary for improving quality of care, but also the skills and knowledge essential to fully participate in the change process associated with quality improvement efforts.
Deploying these rules requires the participation of virtually all stakeholders. Nursing is clearly a key partner in the convening of health profession associations as well as key industry and quality organization representatives to lead this transformation, expand the research underlying the rules, and develop an agenda to examine progress and next steps related to actions supporting the application of this rules set. A total of 7 years has passed since the release of the Quality Chasm report. No doubt progress in health care redesign vis-à-vis the rules set has occurred during this time. However, there is considerably more work to be done in each of these areas.
The Quality Chasm report described the work of health care as being “characterized by more to know, more to manage, more to watch, more to do, and more people involved in doing it at any time in the nation’s history”3 (p. 25). The statement is certainly descriptive of nursing as well. All too familiar to nurses is the growing complexity of both health care and the nature of nursing knowledge and nursing practice. Given these complexities, individual nurses, as with other clinicians, cannot possibly recall and apply all knowledge necessary for the delivery of safe, high-quality patient, family, or community care. The complexity of nursing and medical practice has markedly increased, the technologies are more numerous and complex, and the evidence base underlying practice is rapidly expanding. Recognizing these challenges, the first recommendation in the Quality Chasm report restated the purpose of the health care system as articulated by President Clinton’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry: “All health care organizations, professional groups, and private and public purchasers should adopt as their explicit purpose to continually reduce the burden of illness, injury and disability, and to improve the health and functioning of the people of the United States.”3 (p. 39). In contemplating this statement, nurses might ask what the collective contribution of nursing is and should be to achieving this purpose. How do we pursue this goal? How do we know whether we and other stakeholders in the U.S. health care system are making progress toward achieving it? The Quality Chasm report adds more specificity to this recommendation by setting out six aims (see Table 2). To achieve the aims of the purpose statement articulated above, the Quality Chasm report suggests that these six aims should be the focus of nurses and other clinicians, and should be pursued in all health care settings.
Table 2
IOM’s Six Aims for Improving Health Care Quality
Aim 1—Safe Care
The Quality Chasm noted, “The health care environment should be safe for all patients, in all of its processes, all of the time. This standard of safety implies that organizations should not have different, lower standards of care on nights and weekends or during times of organizational change”3 (p. 45). Recognizing the particular danger that handoffs can pose to patients, the report notes that handoffs are frequently the first place where patient safety is compromised. Clearly, part and parcel of the work of nurses are the transactions that occur among nurses and others as information, components of care processes, and patients themselves are handed off to others. Nursing work is punctuated by patient transfers from one environment to another (e.g., inter- and intra-institutional transfers of patients), from shift to shift, or communication from one clinician to another (e.g., information given by a nurse to different physical therapists caring for the same patient). Moreover, because of their ongoing contact with patients and their families, nurses are in pivotal positions to both inform and incorporate the observations and concerns of these individuals into creating safe care environments. To do so require nurses to consider all information conveyed to them by patients and family members and to encourage that communication.Aim 2—Effective Care
The provision of effective nursing care rests on the development and use of nursing evidence, as well as evidence produced by other disciplines with relevance to nursing practice. Effective care is based on evidence derived from four types of research: laboratory experiments, clinical trials, epidemiological research, and outcomes research, including case reports.3 Outcomes research, critical to improving care quality, uses information about how well interventions work on a large, generalizable scale. Nurse researchers engage in all four types of research, and each type is capable of informing aspects of care delivery and care quality. Nevertheless, there is a paucity of research to undergird the application of many interventions, nursing and non-nursing alike. Looking to the future, the Quality Chasm report suggests that “the knowledge base about effective care and its use in health settings will constantly expand through improved methods of accessing, summarizing and assessing information and making it available at the point of care for the patient”3 (p. 48), Already, information technology systems in some health care settings provide immediate access to clinical guidelines, step-by-step approaches to procedures, and other information that is based on research evidence or, in its absence, expert judgment.In addition to expecting the further development of and adherence to an evidence base, the Quality Chasm report also highlights the importance of nurses and other clinicians systematically and continually reviewing the outcomes of the care that they provide. Currently, care results are rolled up and reflected in overall performance indicators for nursing homes and hospitals. With some exceptions, there is relatively limited information that is currently collected, assessed, and fed back to nurses to help them better understand their individual impact on care quality and thereby assist them in improving their performance. Clearly, efforts that have resulted in the development of nursing indicators are a step in this direction. This is one more important area in which nurses can engage to further the quality improvement agenda.
Aim 3—Patient-Centered Care
Aspects of patient-centered nursing care have long been incorporated in nursing education programs. However, the meaning of the term has evolved and the extent to which it is met is variable. Gerteis and colleagues16 put forward a set of dimensions of patient-centered care, including respect for patients’ values, preferences, and expressed needs; coordination and integration of care; information, communication, and education; physical comfort; emotional support; and involvement of family and friends. Considerable nursing and other research remains to be done to better delineate the outline of this concept and strategies for addressing it. A related concept, population-centered care, is discussed extensively in the IOM report Quality Through Collaboration: The Future of Rural Health. This important concept has even less evidence-based approaches to help guide its achievement.Aim 4—Timely Care
Timeliness of care delivery is often compromised, almost regardless of where a consumer comes in contact with health care. From emergency rooms to schools, nurses see first hand the difficulties in providing timely access to care. Timeliness is compromised when patients needing immediate medical attention find themselves in overcrowded emergency rooms, or individuals without health insurance are delayed in accessing health care or there is a lack of available clinicians. Delays like these are too often the norm. Many factors, both internal and external to the care environment, impact timeliness. Internal to delivery systems, analyzing and refining the actual design of effective processes is overlooked. Instead, the blunt instrument used to drive timeliness is often the expectation for nurses and other clinicians to do more and, in some cases, faster. This approach itself can, at times, compromise care quality.Efforts to improve timeliness are multifaceted. One of the essential tools to address parts of this challenge is technology. The expanded use of call-a-nurse lines, e-mail exchanges between clinicians and patients, and consumer access to telemedicine applications linking rural and urban facilities, are part of the developing technology-based toolkit needed to increase timely access to care.
Aim 5—Efficient Care
Efficiency is not necessarily a hallmark of the U.S. health care system. In fact, some quality experts indicate that adding more financial resources to the health care delivery system is highly inefficient, given the high level of waste in current practices. Since nurses are on the front lines of health care, nurses are well positioned to work within their institutions at the local level as well as through their associations at the national level to develop and promote agendas designed to increase efficiency, ultimately making better use of the significant financial resources currently directed to health care.Additionally, nurse researchers can play an exceedingly important role in achieving efficiency. For example, Naylor17 found that elderly patients receiving a comprehensive intervention delivered by advanced practice nurses (APNs) in the hospital and followed in the home significantly decreased expensive hospitalizations. APN care resulted in average per capita expenditures of $6,152 compared to the control group expenditure of $9,618. As a result, efforts are underway to help move this intervention into the broader practice environment.
As the growth in health care expenditures continues to rise nationally, public policymakers, insurers, and others will be far more open to nursing practice models as well as other strategies that help to rein in high costs while sustaining or improving care quality. Efforts toward achieving this aim provide new opportunities for nurses to create models that maximize the contribution of nursing care and innovation in quality improvement.
Aim 6—Equitable Care
Equity refers to universal access to health care services.3 Challenges surrounding equity are reflected in disparities in health care by ethnic and socioeconomic groups, lack of health insurance or underinsurance, and geographic inequity that influences the services available. Equity as an aim tied to geographic access is discussed later in this section on the IOM report, Quality Through Collaboration: The Future of Rural Health Care.Ten Rules of Health Care Redesign
In addition to advancing a core set of improvement aims, the Quality Chasm report also put forward 10 rules to guide the redesign of health care. The report recommended that this redesign effort incorporate the full complement of health care stakeholders, including patients, payers, clinicians, and others. Many of these rules have underlying evidence to support them. However, some of the rules do not, and in those cases, the report included supporting rationale. The current set of rules that guides health care delivery and the rules proposed to guide the redesign of health care are delineated in Table 3.Table 3
Simple Rules for the 21st Century Health Care System
Regarding new rule four, shared knowledge and free flow of information, Quality Chasm cited evidence that giving patients access to their own health and clinical information improves care processes and health outcomes. Clearly, electronic personal health records and Web-based information have considerable potential to enhance patient knowledge and stimulate healthy behavior. However, there is limited information about how nurses can help patients to fully harness these information resources. Nurses can lead efforts to make these rules actionable across health systems, particularly as they influence the redesign of nursing practice, the nurse-patient relationships, the relationships between nurses and other disciplines, and the relationship of nurses to care processes. Additionally, these expectations should be incorporated into nursing curricula to ensure that nurses are able to engage and support the refinement and application of important features of redesigned health care systems. In the process, nurses learn not just the changes necessary for improving quality of care, but also the skills and knowledge essential to fully participate in the change process associated with quality improvement efforts.
Deploying these rules requires the participation of virtually all stakeholders. Nursing is clearly a key partner in the convening of health profession associations as well as key industry and quality organization representatives to lead this transformation, expand the research underlying the rules, and develop an agenda to examine progress and next steps related to actions supporting the application of this rules set. A total of 7 years has passed since the release of the Quality Chasm report. No doubt progress in health care redesign vis-à-vis the rules set has occurred during this time. However, there is considerably more work to be done in each of these areas.
Much
of the national discussion about the health workforce, particularly
nursing, has focused primarily on supply strategies to address current
and anticipated workforce shortages. However, from a quality improvement
perspective, there is also an imperative to focus on the capacity of
the health care workforce to function in redesigned care systems. The
purpose of the health care system articulated earlier will not be
attained without significant attention to determining and disseminating
the requisite skills and knowledge across the health care workforce. Health Professions Education: A Bridge to Quality8
delineated the needed transformation skills and knowledge of the
various health professions. As with predecessor reports, the call for
change is clear and direct, beginning with the statement, “Education for
the health professions is in need of a major overhaul”8 (p. 1). This assertion and the subsequent observations and recommendations apply to all health professions, including nursing.
The Health Professions Education report described the shortcomings of today’s health professions education programs. Among these shortcomings was the need for individuals to work effectively in interdisciplinary teams—something for which they rarely receive training. That is, “patients and families commonly report that caregivers appear not to coordinate their work or even to know what each other is doing”8 (p. 31). This concern is particularly disconcerting given the increase in chronic disease burden and the clear necessity for collaboration across settings and provider types to meet the needs of patient populations. Another all-too-common educational shortcoming is the lack of an educational foundation in informatics. Future clinical practice will occur in health information technology-rich environments, in spite of the current slow uptake of information technology.8
The vision advanced in Health Professions Education stated, “All health professionals should be educated to deliver patient-centered care as members of an interdisciplinary team, emphasizing evidence-based practice, quality improvement approaches, and informatics”8 (p. 45). Yet gaps exist between the needs and expectations for the workforce in health care environments and the preparation of those professionals in academic environments. This disconnect is highly problematic because, “At the core of a redesigned health care system are health professionals”8 (p. 37). Attention to the educational preparation of the health professions workforce is essential to the meaningful engagement of the entire quality agenda.
Additionally, health systems need to be analyzed to determine the extent to which the systems facilitate or constrain the deployment of skills and knowledge associated with this competency.
Interdisciplinary approaches to research on the set of five competencies may be viewed as too challenging to build in academic environments. Yet it may be in this confluence of ideas, philosophies, and approaches that nurse researchers and others are better able to understand, test, and design interdisciplinary practices. In fact, the hard work of interdisciplinary practice may best be modeled through interdisciplinary education and research efforts that begin in academic environments. The culture of many academic environments, however, does not yet value the production of interdisciplinary education or research partnerships.
Much work remains in terms of teaching the five competencies in nursing education programs, applying the competencies in nursing practice, and focusing on the competencies through nursing research.
The Health Professions Education report gives extensive consideration to the purposes and limitations of accreditation, certification, and licensure and the relationship of these oversight processes to clinician competence and patient outcomes. Currently, most of these oversight processes do not address nurses’ knowledge of any of the five competency areas. As with other disciplines, actually demonstrating competency is generally not part of the ongoing oversight of individual nurses. This report suggested that hard work on the part of oversight bodies (e.g., developing assessment tools) must be done to assure the public that nurses maintain minimum levels of competence throughout their careers.8
There is tremendous pressure on academic programs to ensure that students acquire other essential core content, making the addition of expectations such as those expressed in Health Professions Education difficult to accommodate. Nevertheless, the case is made. The inadequacy of educational preparation is reflected in the lack of skills and knowledge applied in current nursing practice. This report asserts, “The extent to which health professionals are implementing these competency areas does not meet the health care needs of the American public”8 (p. 67).
The Health Professions Education report described the shortcomings of today’s health professions education programs. Among these shortcomings was the need for individuals to work effectively in interdisciplinary teams—something for which they rarely receive training. That is, “patients and families commonly report that caregivers appear not to coordinate their work or even to know what each other is doing”8 (p. 31). This concern is particularly disconcerting given the increase in chronic disease burden and the clear necessity for collaboration across settings and provider types to meet the needs of patient populations. Another all-too-common educational shortcoming is the lack of an educational foundation in informatics. Future clinical practice will occur in health information technology-rich environments, in spite of the current slow uptake of information technology.8
The vision advanced in Health Professions Education stated, “All health professionals should be educated to deliver patient-centered care as members of an interdisciplinary team, emphasizing evidence-based practice, quality improvement approaches, and informatics”8 (p. 45). Yet gaps exist between the needs and expectations for the workforce in health care environments and the preparation of those professionals in academic environments. This disconnect is highly problematic because, “At the core of a redesigned health care system are health professionals”8 (p. 37). Attention to the educational preparation of the health professions workforce is essential to the meaningful engagement of the entire quality agenda.
New Competencies for Health Professionals
The set of five competencies reflected in the vision statement are considered highly applicable to all health care disciplines, including nursing, although the manner in which they are operationalized by each discipline will vary. As with some of the rules for redesign presented in the Quality Chasm report, the evidence base underlying some of these competencies is incomplete and additional research is needed. Where research findings are limited, expert rationale for the competency is provided.Competency 1—Provide patient-centered care
The report noted that patient-centered care includes knowledge of shared responsibility between patients and caregivers; communication approaches that allow patient access to information and achieve patient understanding; consideration of patients’ individuality, values, and needs; and focus on the use of related population-based strategies to improve appropriate use of health services. The Health Professions Education report cites research related to some of these characteristics. For example, findings indicated that patients who were involved in decision making about their care have higher functional status, better outcomes, and lower costs.8Additionally, health systems need to be analyzed to determine the extent to which the systems facilitate or constrain the deployment of skills and knowledge associated with this competency.
Competency 2—Work in interdisciplinary teams
Interdisciplinary teams have been shown to enhance quality and lower costs. Substantially more research is needed to determine characteristics that facilitate team effectiveness, as well as the development of successful academic models capable of teaching and testing these performance attributes. Challenging the development of interdisciplinary educational content and the use of this competency in practice is the absence of a common language across disciplines, politics, and turf battles among the professions. Berwick captured the essence of interdisciplinary practice in a statement he offered in the development of the Health Professions Education report when he said8 (p. 56), “System-mindedness means cooperation…. It means asking yourself … not what are the parts of me, not what do I do, but what am I part of?” For health professions educators, including nursing faculty, a corollary may be how do we help students acquire knowledge about their chosen profession as well as knowledge about how to effectively function in interprofessional teams of which they are destined to become part? Questions for nurse educators include how well are we instilling this competency in students and, how do we know?Interdisciplinary approaches to research on the set of five competencies may be viewed as too challenging to build in academic environments. Yet it may be in this confluence of ideas, philosophies, and approaches that nurse researchers and others are better able to understand, test, and design interdisciplinary practices. In fact, the hard work of interdisciplinary practice may best be modeled through interdisciplinary education and research efforts that begin in academic environments. The culture of many academic environments, however, does not yet value the production of interdisciplinary education or research partnerships.
Competency 3—Employ evidence-based practices
The IOM describes evidence-based practice as the integration of research evidence, clinical expertise, and patient values in making decisions about the care of individual patients. Each of these sources may be contributing factors relevant to decision making regarding patient care. In terms of the implications of this competency for nurses, the report indicated that the following knowledge and skills were necessary: knowing how to find the best sources of evidence, formulating clear clinical questions, and determining when and how to integrate new findings into practice. This knowledge requires bridging content between traditional nursing research courses and clinical courses. The Health Professions Education report noted that the evidence base for nursing and other disciplines is markedly limited, and the availability of data that captures information around nursing interventions in administrative and clinical records for research purposes is minimal. Some nurse researchers and nursing organizations are playing pivotal roles in attempting to address this deficit.Competency 4—Apply quality improvement
The science of quality improvement is expanding rapidly, and the competency of nurses to apply this science is important. Through academic and continuing education opportunities, nurses need to be competent in measuring quality of care, assessing and benchmarking practices to identify improvement opportunities, designing and testing interventions, identifying hazards and errors in care, implementing safety design principles such as standardization and human factors training, and participating as a member of interdisciplinary teams8 (p. 59). A major challenge is the lack of quality improvement content expertise across faculty. Deans, other administrators, and faculty leaders need to focus on acquiring this expertise for their faculty as well as incorporating it into nursing education curricula, including clinical coursework.Competency 5—Utilize informatics
Health care informatics relates to the application of information technology (IT) systems to problems in health care and includes an array of applications from order entry to decision support systems. Research findings indicate that IT applications can enhance patient safety by standardizing, flagging errors, and eliminating handwritten data, among other functions.8 Utilizing informatics can influence knowledge management, communication, and decisionmaking. Educational programming to target facets of this competency have increased in health care environments as well as in academic programs. However, considerable work remains to be done to prepare nurses to fully harness informatics to ensure safety and enhance care quality. Not the least of this work is the analysis of environmental attributes that contribute to successful informatics applications.Much work remains in terms of teaching the five competencies in nursing education programs, applying the competencies in nursing practice, and focusing on the competencies through nursing research.
The Health Professions Education report gives extensive consideration to the purposes and limitations of accreditation, certification, and licensure and the relationship of these oversight processes to clinician competence and patient outcomes. Currently, most of these oversight processes do not address nurses’ knowledge of any of the five competency areas. As with other disciplines, actually demonstrating competency is generally not part of the ongoing oversight of individual nurses. This report suggested that hard work on the part of oversight bodies (e.g., developing assessment tools) must be done to assure the public that nurses maintain minimum levels of competence throughout their careers.8
There is tremendous pressure on academic programs to ensure that students acquire other essential core content, making the addition of expectations such as those expressed in Health Professions Education difficult to accommodate. Nevertheless, the case is made. The inadequacy of educational preparation is reflected in the lack of skills and knowledge applied in current nursing practice. This report asserts, “The extent to which health professionals are implementing these competency areas does not meet the health care needs of the American public”8 (p. 67).
The
last IOM report presented in this section addressed the unique
circumstances of rural health care—rural populations and characteristics
that influence the quality of rural health care. Based on a review of
research findings as well as expert opinion, a number of specific
recommendations are offered that build on rural health strengths and
address their challenges. The IOM’s Quality Through Collaboration: The Future of Rural Health
highlighted a conclusion important to nurses and others: that is, there
is a paucity of research available on the quality of rural health care.
As with urban health care, the limited rural research that does exist
indicates variability of care quality.11
This circumstance underscores the need for nurses and others with
interest and expertise in rural health to further expand knowledge in
this largely ignored area. One particular area needing nursing inquiry
is the extent to which rural health care delivery reflects activity and
progress toward achieving the six aims for improvement.
A unique contribution of the Future of Rural Health report is the application of the six aims to improve not just care quality delivered in health care organizations, as has been discussed in earlier reports, but also to target efforts that can improve the quality of health in the general population. Nurses in rural communities can be pivotal in helping to build a local community focus on both the quality of health and the quality of health care. The report provides illustrative examples of the application of each of the six aims and community level interventions to achieve those aims. Much of the work of targeting efforts toward improving the quality of population health will involve nurses and other leaders in rural health care settings working with community leaders in local schools, government, and other sectors. How to effectively engage this collective focus to advance population health should be a priority research area.
As with most of the reports in the IOM Quality Chasm series, the theme of leadership emerged in The Future of Rural Health. In this case, particular attention is given to the need for rural health system leaders to embrace and drive quality improvement within their organizations as well as the need to engage larger issues of population health quality. An identified strength of many rural communities is the familiarity that people have with each other and the various local community sectors. Also, often typical of rural communities is the orientation and practice of engaging across sectors to achieve community-level outcomes. This characteristic can help to facilitate new efforts around building quality into population health.11
The Future of Rural Health report pivots from the major components of the Crossing the Quality Chasm report and frames the issues in a rural context. For example, priority issues such as information technology applications, quality improvement infrastructure components, workforce considerations, and the aims for improvement are all viewed through the prism of a rural context. In addition, The Future of Rural Health cited relevant rural examples of each of the six aims, considering them in the context of the community as well as the context of health care delivery. Measures of the safety aim included measuring community characteristics such as occupational accident rates in rural areas and toxic environmental exposure/risk from pesticides. Brief discussions focused on community-level strategies for improving safety, effectiveness in community health improvement, and community-centered care that reflects responsiveness to the aggregated needs, values, and other characteristics of the local community. Clearly, the broadened application of the six aims for improvement in a rural community context offers an area for research and reconfigured interdisciplinary efforts that include stakeholders outside of traditional health care settings. The community-level application of the six aims, revamped to consider unique characteristics of urban areas, also should be highly relevant to urban communities and populations.
Too frequently, research conducted on quality and safety interventions in urban health care settings has been directly generalized to the often very different environments, staffing mix, and patient populations found in rural health care settings. For example, deploying rapid response teams in rural areas needs to take into consideration the different staff mix available on site in rural settings. Relevant research on functions common to rural health care settings is extremely limited. For example, there is minimal nursing research on the processes involved in patient stabilization and transfer. This is a set of activities common to rural hospitals but far less frequently performed in urban hospitals. Research on patient outcomes associated with these processes is virtually nonexistent. More efforts need to be directed toward developing and determining relevant rural knowledge and tools, appropriate performance measures, and the development of data feedback capabilities. To begin to fill knowledge gaps and improve health care quality and population health, access to the science of quality improvement and acquiring related expertise is pivotal. This includes acquiring competence in evaluating, adopting, and adapting this new knowledge area for application in rural environments.18
In addition to identifying gaps in research knowledge and new framing of aims for application to quality improvement in rural population health, the Future of Rural Health report also addressed internal and external drivers of quality improvement specific to rural health systems. For example, unlike most urban hospitals, which are reimbursed through the prospective payment system, a large subset of rural hospitals are designated as critical access hospitals. These hospitals receive cost-based reimbursement, and there are currently no requirements linking Medicare payment to reporting on quality indicators, as is the case with prospective payment system hospitals. The report states that no providers, rural or urban, should be excluded from public reporting. However, mechanisms for linking cost-based reimbursement to quality indicators and eventually patient outcomes need to be developed for rural health care facilities. Additionally, determining how best to report and assign meaning to data extracted from small numbers of patient encounters remains a challenge.
In terms of drivers internal to rural health care settings, the job design of nurse leaders typically requires them to manage multiple roles and expectations. For example, frequently, the nurse responsible for quality assurance and improvement in a facility carries many other responsibilities as well. Given the limited numbers of nurses and other personnel in rural communities, efficiently acquiring and applying quality improvement knowledge and related skills can be particularly challenging. Conversely, because health care providers tend to be relatively few in number, information and new care approaches are often rapidly diffused throughout small rural facilities.
The report devoted significant attention to characteristics essential to the rural health care workforce. Building on the Health Professions Education report, The Future of Rural Health noted that the five identified competencies are all relevant to rural health care, but the applications may be different. Interdisciplinary teams may consist of individuals geographically separated, but who share involvement in the ongoing care of individuals. Electronic intensive care units are an example. Under these circumstances, applying team concepts may have special ramifications for nurses and others. While research findings from some of these practices indicated markedly improved patient morbidity and mortality, there was virtually no research base on which to guide the configuration and deployment of these types of teams.
The Future of Rural Health also advocated for educational preparation that includes rural-relevant practice knowledge and rural clinical experience. The role of rural consumers in acquiring quality care is also discussed, with attention given to the fact that their role in managing their health may be operationalized differently compared to their urban counterparts given resource availability, etc. For example, access to certain clinicians, including home health nurses and diabetes nurse educators, may be enabled through Web and other technology applications. Yet minimal study of the quality of these encounters has been undertaken. Although technology offers the promise of linking sparsely populated areas to health care services, there is a digital divide between rural and urban areas across the country. To the extent that electronic connectivity is essential for care continuity, special effort needs to be made to overcome these challenges. Public policy is and will continue to play a major role in bridging this divide, offering nurses another area to engage in issues concerning rural access to quality health care.
A unique contribution of the Future of Rural Health report is the application of the six aims to improve not just care quality delivered in health care organizations, as has been discussed in earlier reports, but also to target efforts that can improve the quality of health in the general population. Nurses in rural communities can be pivotal in helping to build a local community focus on both the quality of health and the quality of health care. The report provides illustrative examples of the application of each of the six aims and community level interventions to achieve those aims. Much of the work of targeting efforts toward improving the quality of population health will involve nurses and other leaders in rural health care settings working with community leaders in local schools, government, and other sectors. How to effectively engage this collective focus to advance population health should be a priority research area.
As with most of the reports in the IOM Quality Chasm series, the theme of leadership emerged in The Future of Rural Health. In this case, particular attention is given to the need for rural health system leaders to embrace and drive quality improvement within their organizations as well as the need to engage larger issues of population health quality. An identified strength of many rural communities is the familiarity that people have with each other and the various local community sectors. Also, often typical of rural communities is the orientation and practice of engaging across sectors to achieve community-level outcomes. This characteristic can help to facilitate new efforts around building quality into population health.11
The Future of Rural Health report pivots from the major components of the Crossing the Quality Chasm report and frames the issues in a rural context. For example, priority issues such as information technology applications, quality improvement infrastructure components, workforce considerations, and the aims for improvement are all viewed through the prism of a rural context. In addition, The Future of Rural Health cited relevant rural examples of each of the six aims, considering them in the context of the community as well as the context of health care delivery. Measures of the safety aim included measuring community characteristics such as occupational accident rates in rural areas and toxic environmental exposure/risk from pesticides. Brief discussions focused on community-level strategies for improving safety, effectiveness in community health improvement, and community-centered care that reflects responsiveness to the aggregated needs, values, and other characteristics of the local community. Clearly, the broadened application of the six aims for improvement in a rural community context offers an area for research and reconfigured interdisciplinary efforts that include stakeholders outside of traditional health care settings. The community-level application of the six aims, revamped to consider unique characteristics of urban areas, also should be highly relevant to urban communities and populations.
Too frequently, research conducted on quality and safety interventions in urban health care settings has been directly generalized to the often very different environments, staffing mix, and patient populations found in rural health care settings. For example, deploying rapid response teams in rural areas needs to take into consideration the different staff mix available on site in rural settings. Relevant research on functions common to rural health care settings is extremely limited. For example, there is minimal nursing research on the processes involved in patient stabilization and transfer. This is a set of activities common to rural hospitals but far less frequently performed in urban hospitals. Research on patient outcomes associated with these processes is virtually nonexistent. More efforts need to be directed toward developing and determining relevant rural knowledge and tools, appropriate performance measures, and the development of data feedback capabilities. To begin to fill knowledge gaps and improve health care quality and population health, access to the science of quality improvement and acquiring related expertise is pivotal. This includes acquiring competence in evaluating, adopting, and adapting this new knowledge area for application in rural environments.18
In addition to identifying gaps in research knowledge and new framing of aims for application to quality improvement in rural population health, the Future of Rural Health report also addressed internal and external drivers of quality improvement specific to rural health systems. For example, unlike most urban hospitals, which are reimbursed through the prospective payment system, a large subset of rural hospitals are designated as critical access hospitals. These hospitals receive cost-based reimbursement, and there are currently no requirements linking Medicare payment to reporting on quality indicators, as is the case with prospective payment system hospitals. The report states that no providers, rural or urban, should be excluded from public reporting. However, mechanisms for linking cost-based reimbursement to quality indicators and eventually patient outcomes need to be developed for rural health care facilities. Additionally, determining how best to report and assign meaning to data extracted from small numbers of patient encounters remains a challenge.
In terms of drivers internal to rural health care settings, the job design of nurse leaders typically requires them to manage multiple roles and expectations. For example, frequently, the nurse responsible for quality assurance and improvement in a facility carries many other responsibilities as well. Given the limited numbers of nurses and other personnel in rural communities, efficiently acquiring and applying quality improvement knowledge and related skills can be particularly challenging. Conversely, because health care providers tend to be relatively few in number, information and new care approaches are often rapidly diffused throughout small rural facilities.
The report devoted significant attention to characteristics essential to the rural health care workforce. Building on the Health Professions Education report, The Future of Rural Health noted that the five identified competencies are all relevant to rural health care, but the applications may be different. Interdisciplinary teams may consist of individuals geographically separated, but who share involvement in the ongoing care of individuals. Electronic intensive care units are an example. Under these circumstances, applying team concepts may have special ramifications for nurses and others. While research findings from some of these practices indicated markedly improved patient morbidity and mortality, there was virtually no research base on which to guide the configuration and deployment of these types of teams.
The Future of Rural Health also advocated for educational preparation that includes rural-relevant practice knowledge and rural clinical experience. The role of rural consumers in acquiring quality care is also discussed, with attention given to the fact that their role in managing their health may be operationalized differently compared to their urban counterparts given resource availability, etc. For example, access to certain clinicians, including home health nurses and diabetes nurse educators, may be enabled through Web and other technology applications. Yet minimal study of the quality of these encounters has been undertaken. Although technology offers the promise of linking sparsely populated areas to health care services, there is a digital divide between rural and urban areas across the country. To the extent that electronic connectivity is essential for care continuity, special effort needs to be made to overcome these challenges. Public policy is and will continue to play a major role in bridging this divide, offering nurses another area to engage in issues concerning rural access to quality health care.
In
summary, the Quality Chasm series of reports emphasized a number of key
attributes of the architecture needed to build a safe, consistently
high-performing health care system. Expressed throughout the reports
were serious concerns about the status of contemporary health care.
Essential features of high-quality care systems—such as workforce
competencies, effective application of internal and external drivers,
progress toward achieving the six identified aims for improvement, and
the application of a set of rules to systems redesign—are far from where
they should be. The Quality Chasm series called for leadership in
education, practice, and research to drive needed change. The series
called for major overhaul of not just the organizations in which health
care providers work, but the education of health care providers
themselves. The series made a special effort to recognize the unique
needs of specific populations, such as those in rural communities or
those with mental health problems, and recommended approaches to more
effectively deliver quality care to those populations. Based on the
challenges and recommendations set forth, it is clear that significant
work remains to be done.
Specific to the nursing profession, nurse educators, clinicians, and researchers need to help build state-of-the-art and state-of-the-science approaches for redesigning nursing care processes, using information technology between nurses and patients and nurses and other clinicians; acquiring, managing, and appropriately applying new knowledge and skills; preparing nurses to function effectively in teams; and evaluating nurses’ performance in this regard. Regardless of the settings in which nurses practice, much more effort must be devoted to care coordination for individuals with chronic conditions, while diligently measuring both performance and outcomes. Nurses have a substantive and essential role in helping to apply the quality framework articulated in the IOM Quality Chasm series. And nurses clearly have a role in developing additional approaches and new features to the quality agenda. Active engagement in patient safety and quality improvement efforts is relevant to all nurses. Unlike the minimal progress from Nightingale’s time until now, hopefully future nurses will be able to reflect back to the beginning of the 21st century and determine that nursing made significant strides. They will see improvement in both the quality of health and health care quality due to an improved role of nurses in providing quality care.
Specific to the nursing profession, nurse educators, clinicians, and researchers need to help build state-of-the-art and state-of-the-science approaches for redesigning nursing care processes, using information technology between nurses and patients and nurses and other clinicians; acquiring, managing, and appropriately applying new knowledge and skills; preparing nurses to function effectively in teams; and evaluating nurses’ performance in this regard. Regardless of the settings in which nurses practice, much more effort must be devoted to care coordination for individuals with chronic conditions, while diligently measuring both performance and outcomes. Nurses have a substantive and essential role in helping to apply the quality framework articulated in the IOM Quality Chasm series. And nurses clearly have a role in developing additional approaches and new features to the quality agenda. Active engagement in patient safety and quality improvement efforts is relevant to all nurses. Unlike the minimal progress from Nightingale’s time until now, hopefully future nurses will be able to reflect back to the beginning of the 21st century and determine that nursing made significant strides. They will see improvement in both the quality of health and health care quality due to an improved role of nurses in providing quality care.
Every
report in the Quality Chasm series calls for specific, targeted
research to further develop the evidence base related to quality care.
Research targeting quality improvement has been supported and
implemented by various stakeholders, ranging from health profession
organizations to Federal agencies to health providers themselves.
Findings and implications are being applied in a variety of ways, from
changing internal drivers of quality such as work structure (e.g., rapid
response teams) to altering external drivers of quality (e.g., paying
providers for performance based on evidence-based quality indicators).
While nurses have been part of many of the research activities,
significant research remains to be done.
The following is a compilation of some of the exemplar areas of research derived from the four reports reviewed in this section. These research areas are both relevant to nursing and are areas for which nursing’s contribution is important.
The following is a compilation of some of the exemplar areas of research derived from the four reports reviewed in this section. These research areas are both relevant to nursing and are areas for which nursing’s contribution is important.
- The role of leaders in addressing errors and designing safety and quality into health care systems is a common thread throughout the IOM Quality Chasm report series. Currently, the work design of practice in clinical settings introduces significant potential for executing unsafe actions. This is particularly relevant to nursing, given that much of the care delivered in health systems is nursing care.
- Public, standardized reporting of serious medical errors is recommended, and a number of States have implemented error reporting systems. Recently, Federal legislation related to reporting errors has been enacted.
- Encourage health care consumers to actively participate in ensuring the delivery of safe care.
- Using external factors such as paying for quality performance can drive quality improvement. Examples exist of health systems that have tested the intervention of using payment incentives to improve performance (e.g., Premier demonstration project funded by the Centers for Medicare & Medicaid Services).
- Creating learning environments is a prerequisite to systemwide delivery and improvement of care quality.
- Even when evidence exists regarding effective approaches to care delivery, this information is not consistently applied.
- The Quality Chasm report series proposes a set of new rules to guide health care systems, including rules such as the need for transparency, anticipation of patient needs, and the patient as the source of control.
- Population-centered care is a concept central to The Future of Rural Health: In this report the six aims for improvement discussed in many of the other IOM reports were considered in a population rather than a health care system context. However, an evidence base needs to be developed to better understand how to construct this concept for the purpose of improving health and health care.
- The Future of Rural Health discusses the importance of linking facilities and providers across geographic distances as a means to build efficient quality improvement infrastructure. Connecting clinicians using IT to provide access to locally unavailable care has been implemented in terms of telemental health, e-Intensive Care, and other IT-based services.
- The Health Professions Education report advances five competencies considered essential to the ability of providers to deliver high-quality care.
- 1.
- Quality first: better health care for all Americans. Washington, DC: U.S. Government Printing Office; 1998. The President’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry.
- 2.
- Kohn LT, Corrigan JM, Donaldson MS, editors. A report of the Committee on Quality of Health Care in America, Institute of Medicine. Washington, DC: National Academy Press; 2000. To err is human: building a safer health system.
- 3.
- Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press; 2001.
- 4.
- Nightingale F. Notes on hospital. London: John W. Parker and Son, West Strand; 1859.
- 5.
- Institute of Medicine. Leadership by example: coordinating government roles in improving health care quality. Washington, DC: National Academies Press; 2002.
- 6.
- Institute of Medicine. Fostering rapid advances in health care: learning from systems demonstrations . Washington, DC: National Academies Press; 2002.
- 7.
- Institute of Medicine. Priority areas for national action: transforming health care quality . Washington, DC: National Academies Press; 2003.
- 8.
- Institute of Medicine. Health professions education: a bridge to quality . Washington, DC: National Academies Press; 2003.
- 9.
- Institute of Medicine. Patient safety: achieving a new standard for care . Washington, DC: National Academies Press; 2003.
- 10.
- Institute of Medicine. Keeping patients safe: transforming the work environment of nurses . Washington, DC: National Academies Press; 2004.
- 11.
- Institute of Medicine. Quality through collaboration: the future of rural health . Washington, DC: National Academies Press; 2005.
- 12.
- Institute of Medicine. Preventing medication errors: quality chasm series . Washington, DC: National Academies Press; 2006.
- 13.
- Institute of Medicine. Improving the quality of health care for mental and substance-use conditions: quality chasm series . Washington, DC: National Academies Press; 2006.
- 14.
- Joint Commission on Accreditation of Healthcare Organization. National patient safety goals [Online] 2005. May [Accessed May 3, 2006]. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsg_facts.
- 15.
- Berwick DM, Calkins DR, McCannon CJ, et al. The 100,000 lives campaign: setting a goal and a deadline for improving health care quality. Institute for Healthcare Improvement [Online] 2006. Jan [Accessed May 2, 2006]. Available at: http://www.ihi.org/IHI/Topics/Improvement/ImprovementMethods/Literature/100000LivesCampaignSettingaGoalandaDeadline.html.
- 16.
- Gerteis M, Edgman-Levitan S, Daley J. Understanding and promoting patient-centered care. San Francisco, CA: Jossey-Bass; 1993. Through the patient’s eyes.
- 17.
- Naylor M. Making the business case for the APN care model. Report to the Commonwealth Fund. 2003 Oct;
- 18.
- Coburn AF, Wakefield M, Casey M, et al. Assuring rural hospital patient safety: what should be the priorities? J Rural Health. 2004 Fall;20:314–26. [PubMed]
Source :http://www.ncbi.nlm.nih.gov/books/NBK2677/

No comments:
Post a Comment